| ||||||||||||||
 |
Sutures
BackgroundA surgical suture is used to close the edges of a wound or incision and to repair damaged tissue. There are many kinds of sutures, with different properties suitable for various uses. Sutures can be divided into two main groups: absorbable and non-absorbable. An absorbable suture decomposes in the body. It degrades as a wound or incision heals. A non-absorbable suture resists the body's attempt to dissolve it. Non-absorbable sutures may be removed by a surgeon after a surface incision has healed. Sutures are made from both man-made and natural materials. Natural suture materials include silk, linen, and catgut, which is actually the dried and treated intestine of a cow or sheep. Synthetic sutures are made from a variety of textiles such as nylon or polyester, formulated specifically for surgical use. Absorbable synthetic sutures are made from polyglycolic acid or other glycolide polymers. Most of the synthetic suture materials have proprietary names, such as Dexon and Vicryl. The water-resistant material Goretex has been used for surgical sutures, and other sutures are made from thin metal wire. Sutures are also classified according to their form. Some are monofilaments, that is, consisting of only one thread-like structure. Others consist of several filaments braided or twisted together. Surgeons choose which type of suture to use depending on the operation. A monofilament has what is called low tissue drag, meaning it passes smoothly through tissue. Braided or twisted sutures may have higher tissue drag, but are easier to knot and have greater knot strength. Braided sutures are usually coated to improve tissue drag. Other sutures may have a braided or twisted core within a smooth sleeve of extruded material. These are known as pseudo-monofilaments. A suture can also be classified according to its diameter. In the United States, suture diameter is represented on a scale descending from 10 to 1, and then descending again from 1-0 to 12-0. Suture manufacturing comes under the regulatory control of the Food and Drug Administration (FDA) because sutures are classified as medical devices. Manufacturing guidelines and testing for the industry is provided by a non-profit, non-governmental agency called United States Pharmacopeia, located in Rockville, Maryland.
HistoryPhysicians have used sutures for at least 4,000 years. Archaeological records from ancient Egypt show that Egyptians used linen and animal sinew to close wounds. In ancient India, physicians used the heads of beetles or ants to effectively staple wounds shut. The live creatures were affixed to the edges of the wound, which they clamped shut with their pincers. Then the physician cut the insects' bodies off, leaving the jaws in place. Other natural materials doctors used in ancient times were flax, hair, grass, cotton, silk, pig bristles, and animal gut. Though the use of sutures was widespread, sutured wounds or incisions often became infected. Nineteenth century surgeons preferred to cauterize wounds, an often ghastly process, rather than risk the patient's death from infected sutures. The great English physician Joseph Lister discovered disinfecting techniques in the 1860s, making surgery much safer. Lister soaked catgut suture material in phenol making it sterile, at least on the outside. Lister spent over 10 years experimenting with catgut, to find a material that was supple, strong, sterilizable, and absorbable in the body at an adequate rate. A German surgeon made advances in the processing of catgut early in the twentieth century, leading to a truly sterile material. Catgut was the staple absorbable suture material through the 1930s, while physicians used silk and cotton where a non-absorbable material was needed. Suture technology advanced with the creation of nylon in 1938 and of polyester around the same time. As more man-made textiles were developed and patented for suture use, needle technology also advanced. Surgeons began using an atraumatic needle, which was pressed or crimped onto the suture. This saved the trouble of threading the needle in the operating room, and allowed the entire needle diameter to remain roughly the same size as the suture itself. In the 1960s, chemists developed new synthetic materials that could be absorbed by the body. These were polyglycolic acid and polylactic acid. Previously, absorbable sutures had to be made from the natural material catgut. Synthetic absorbable suture material is now far more prevalent than catgut in United States hospitals. The FDA began requiring approval of new suture material in the 1970s. A Medical Device Amendment was added to the FDA in 1976, and suture manufacturers have been required to seek pre-market approval for new sutures since that time. Manufacturers must comply with specific Good Manufacturing Practices, and guarantee that their products are safe and effective. Patents for new suture materials are granted for 14 years.
Raw MaterialsNatural sutures are made of catgut or reconstituted collagen, or from cotton, silk, or linen. Many countries do no longer accept the use of catgut or reconstituted collagen sutures because of the problems with animal protein products. Synthetic absorbable sutures may be made of polyglycolic acid, a glycolide-lactide copolymer; or polydioxanone, a copolymer of glycolide and trimethylene carbonate. These different polymers are marketed under specific trade names. Synthetic nonabsorbable sutures may be made of polypropylene, polyester, polyethylene terephthalate, polybutylene terephthalate, polyamide, different proprietary nylons, or Goretex. Some sutures are also made of stainless steel. Sutures are often coated, especially braided or twisted sutures. They may also be dyed to make them easy to see during surgery. Only FDA approved dyes and coatings may be used. Some allowable dyes are: logwood extract, chromium-cobalt-aluminum oxide, ferric ammonium citrate pyrogallol, D&C Blue No. 9, D&C Blue No. 6, D&C Green No. 5, and D&C Green No. 6. The coatings used depend on whether the suture is absorbable or non absorbable. Absorbable coatings include Poloxamer 188 and calcium stearate with a glycolide-lactide copolymer. Nonabsorbable sutures may be coated with wax, silicone, fluorocarbon, or polytetramethylene adipate. Suture needles are made of stainless or carbon steel. The needles may be nickel-plated or electroplated. Packaging material includes water-resistant foil, such as aluminum foil, as well as cardboard and plastic.
DesignSutures are designed to meet many different needs. Sutures for abdominal surgery, for example, are different from sutures used in cataract surgery. Since no one type of suture is ideal for every operation, surgeons and medical designers have come up with sutures with varying qualities. One may be more absorbable but less flexible, while another is exceedingly strong but perhaps somewhat difficult to knot. This gives surgeons many options. Designers of a new suture have to take into account many factors. The rate the suture degrades is important, not only along the length of the suture but at the knot. Some sutures need to be elastic, so that they will stretch and not break. Others need to hold tight. Suture manufacturers use specially designed machines to test and study sutures. New suture designs are also tested by subjecting them to chemical tests, such as soaking them in various solutions, and testing on animals.
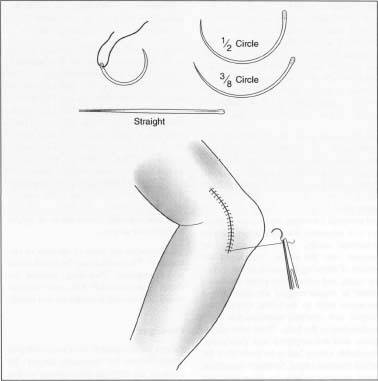
An example of a person being sutured.
The Manufacturing ProcessThe manufacturing of sutures for surgical use is not very different from the production of other synthetic textiles. The raw material is polymerized, and the polymer extruded into fiber. The fiber is stretched and braided on machines similar to ones that might be found in a factory producing polyester thread for the garment industry. The manufacturing process typically occurs at three sites: one plant produces the suture textile, another produces the needles, and a third plant called the finishing plant attaches needles to the sutures, packages, and sterilizes.
Quality ControlSutures, as medical devices, are subject to strict quality control. All the raw materials that arrive at the manufacturing plant are tested to make sure they are what they are supposed to be. Each batch of sutures is tested after the main manufacturing steps for a variety of physical characteristics such as diameter and strength. The suture industry has developed an array of sophisticated instruments for testing special suture characteristics such as knot security and tissue drag. Tests for diameter, length, and strength of the suture are also performed at the finishing plant. The finishing plant must also test how well the needle is attached to the suture. Guidelines for suture quality control are laid down by the independent organization United States Pharmacopeia.
The FutureNew sutures are being developed all the time, to better respond to particular surgical needs. While not replacing sutures, scientists have also devised alternative methods of wound closure. The first surgical stapler was invented in 1908, but stapler technology developed considerably in the 1990s. Precise machines are able to place absorbable staples, as thin as four human hairs, beneath the top layer of skin to secure an incision with minimal scarring. A related device, first tested on patients in the United States in 2000, is a surgical zipper. A surgeon can place the zipper over a straight incision and zip the wound closed, eliminating the need for suturing. After the wound heals, the patient can wash the zipper off in the shower. Another surgical closure method that is still evolving is surgical glue. Surgical glue is less painful than sutures if a wound must be closed without anesthetic. The glue may leave less scarring in some cases, and be easier to care for post-operatively.
| |||||||||||||
![]()
| Be notified of page updates |
wwwswicofilcom2015